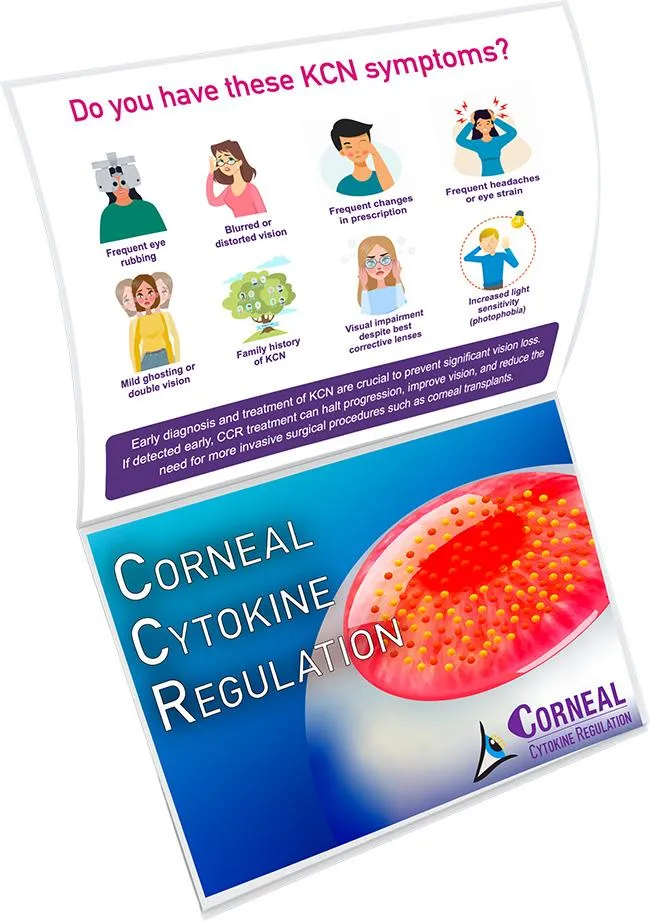
Discover A NEW treatment option for keratoconus (KCN)
Corneal Cytokine Regulation (CCR) Stops KCN Progression and Improves Vision.
No Surgery - Scientifically Evaluated
Know The FACTS
INFLAMMATION LEADS TO KCN
KCN is an inflammatory disorder of the eyes, and treating ocular inflammation stops KCN progression and initiates the vision recovery process.
DID YOU KNOW?
Recent scientific research has clearly shown KCN to be an ocular inflammatory condition due to cytokines produced as part of the body's immune response.
By controlling and eliminating cytokines and ocular inflammation and its associated cofactors, we can stop the KCN progression and reverse the condition.
If inflammation in your eye isn't being treated, the underlying cause of your KCN remains untreated, which may lead to the progression of your KCN .
WHAT IS CCR?
Corneal Cytokine Regulation (CCR) is a ground breaking treatment shown to reduce and regulate cytokines and ocular inflammation and its associated cofactors using acupuncture and herbal medicine.
CCR exhibits the following multi-component, multi-pathway and multi-targeted synergistic mechanism of action for treatment of KCN.
Reduce Cytokines
Reduce Ocular Inflammation
Reduce Oxidative Stress
Reduce Ferroptosis
Improve Ocular Blood Flow
Reduce Ocular Excitotoxcity
Supply Neurotrophins
Supply Antioxidants
CCR offers several compelling advantages for KCN patients compared to conventional treatments.

Halts Progressions of KCN
By eliminating ocular inflammation and its co-factors, the progressions of KCN can be halted

Reversal of Keratoconus
As the cornea heals from ocular inflammation and its associated co-factors are addressed, the cornea starts to heal and reshape.

Improved Visual Acuity
All KCN patients have shown to have improvement in visual acuity. Our standard of "Normal Vision" is 20/15not 20/20.

Myopic Improvements
Keratoconus patients with myopia see an improvement in visual acuity and a reduction in prescription power.

Dry Eye Improvement
Patients with dry eyes experience improved comfort due to a reduction in dry eye symptoms.

Avoid Surgery
Prevent complications arising from surgical treatments such as corneal rejection, corneal scarring, ulcerative keratitis, and glaucoma.

Halts Progression of KCN
By eliminating ocular inflammation and its co-factors, the progression of KCN can be halted

Reversal of KCN*
As the cornea heals from ocular inflammation and its associated co-factors are addressed, the cornea starts to heal and reshape.

Improved Visual Acuity
All KCN patients have shown to have improvement in visual acuity. Our standard of "Normal Vision" is 20/15 not 20/20.

Myopic Improvements
Keratoconus patients with myopia see an improvement in visual acuity and a reduction in prescription power.

Dry Eye Improvement
Patients with dry eyes experience improved
comfort due to a reduction
in dry eye symptoms.

Avoid Surgery
Prevent complications
arising from surgical treatments such as corneal rejection, corneal scarring, ulcerative keratitis, and glaucoma.
*Reversal may have limitations when there is corneal scarring or hydrops due to anatomical damage to cornea.

Halts Progressions of KCN
By eliminating ocular inflammation and its co-factors, the progressions of KCN can be halted
Reversal of Keratoconus
As ocular inflammation and related factors are addressed, the cornea begins to heal and reshape.

Improved Visual Acuity
All KCN patients have shown improved visual acuity. Our standard for "Normal Vision" is 20/15, not 20/20.
Myopic Improvements
Keratoconus patients with myopia see an improvement in visual acuity and a reduction in prescription power.
Dry Eye Improvement
Patients with dry eyes experience improved comfort due to a reduction in dry eye symptoms.
Avoid Surgery
Prevent issues such as corneal rejection, scarring, keratitis, and glaucoma post-surgery.
CCR exhibits multi-component, multi-pathway and multi-target synergistic mechanism of action for treatment of KCN.

“ My vision improved by 8 lines to 20/30 without the need for sclarel lenses. ”
I was surprised to find that I had significant improvement in my vision within 3 weeks of CCR treatment. With both eyes, my vision had improved to 20/30 without the need to use scleral lenses or glasses.
The staff here were very pleasant and made me feel comfortable during the treatment procedure.
- VEERAL - STUDENT
Know The FACTS
Cross-Linking & KCN
Corneal Collagen Cross-linking (CXL) does not reverse damage already done by KCN; it prevents further deterioration.
Upto 22% of patients continue to have KCN progression even after CXL since the ocular inflammation remains untreated.

20/15
Our standards of normal version is beyond 20/20
Most patients achieve 20/15 vision after successfully completing their first round of CCR treatment. About 20% can even read a few letters on the 20/10 line.
CCR revitalizes retinal nerve cells. improving their function and enhancing visual clarity and acuity.

Download CCR Brochure
HEAR FROM OUR PATIENTS
Keratoconus - Advanced Stage - Vision Restored
Keratoconus - Advanced Stage
Vision Restored
Keratoconus and Myopia - Vision Restored
Keratoconus and Myopia
Vision Restored
MOST ASKED QUESTIONS
Why Corneal Cytokine Regulation (CCR) is not covered by my insurance?
Corneal Cytokine Regulation (CCR) is a holistic therapy which uses Traditional Chinese Medicine (TCM) consisting of acupuncture and herbal supplements for treatment of keratoconus.
Holistic therapies such as acupuncture and herbal medicines to treat chronic ocular inflammation are not covered by insurance.
Why is my eye doctor saying keratoconus is not an inflammatory disease?
Many eye doctors historically classified keratoconus (KCN) as a non-inflammatory disease due to outdated medical training, limited diagnostic tools, and early research biases.
However multiple recent research have shown the cause of KCN to be inflammatory. To bridge the gap, consider these questions and provide your doctor with the research articles given under our References section.
-- "Have you tested my tear cytokines (e.g., MMP-9) for inflammation?"
-- "Could my allergies/dry eye be contributing to KC progression?"
-- "Are there anti-inflammatory options (e.g., immunomodulators) for my case?"
Can keratoconus be cured?
By treating the root cause of the keratoconus ie. chronic ocular inflammatory condition, keratoconus can said to be considered cured from its causative factor. However please be aware that not all of the damage caused by keratconus which is irregular astigmatism, thinning of corneal tissue, corneal ectasia and corneal scarring will be reversed.
Are there new treatments for keratoconus to treat root cause and reverse the condition?
Corneal Cytokine Regulation therapy has shown to treat keratoconus by reducing ocular inflammation and improve vision by reversing some of the damage caused by keratoconus.
Is Corneal Cytokine Regulation (CCR) treatment FDA approved?
Corneal Cytokine Regulation is a holistic therapy which uses Traditional Chinese Medicine (TCM) consisting of acupuncture and herbal supplements for treatment of keratoconus. Acupuncture and herbal treatments offered by Traditional Chinese Medicine (TCM) are not subject to FDA approval.
How fast does keratoconus progress?
KCN progression is unpredictable but often has rapid progression in young patients. Early diagnosis and treatments such as Corneal Cytokine Regulation and corneal cross-linking (CXL) are key to avoiding progression and avoid severe vision loss.
Does corneal cross-linking (CXL) reverse keratoconus?
No, corneal cross-linking (CXL) does not reverse keratoconus—it halts progression by strengthening the cornea but cannot restore lost vision or flatten the cone shape.
What percentage of cases has shown progression of keratoconus even after Corneal cross-linking (CXL)?
Studies indicate that upto 22% of keratoconus (KCN) cases show continued progression after corneal cross-linking (CXL), even if the procedure was technically successful. This could be due to the fact that the underlying chronic ocular inflammation still exists and was never treated.
Is keratoconus hereditary?
Yes, keratoconus (KCN) has a strong hereditary component, but genetics alone don’t determine its development. Only 10-20% of KC patients have a close relative with the condition. Even with genetic risk, other environmental factors may be needed to trigger KCN. KC is multifactorial - genes load the gun, but environment pulls the trigger.
When is a corneal transplant needed?
A corneal transplant (keratoplasty) becomes necessary in advanced keratoconus (KCN) when other treatments fail to preserve vision or comfort.
A transplant is only considered when vision is uncorrectable and corneal integrity is compromised. Most KCN patients never need one with early diagnosis of KCN and treating the root cause of KCN i.e ocular inflammation through CCR and corneal cross-linking (CXL).
REFERENCES
-
Increased inflammatory mediators in the ocular surface tissue in keratoconus – Albert Santos, José APM Filho et al.
Summary: The Interleukin-5 (IL-5) and Interleukin-6 (IL-6) cytokines were higher in the corneal epithelium of the keratoconus group, indicating increased inflammation in ocular tissues. Greater immune activity was observed in the corneal and conjunctival epithelial cells of keratoconus patients based on IL-5 and IL-6 gene expression. -
Increased lacrimal inflammatory mediators in patients with keratoconus – Gustavo Souza Moura, Albert Santos et al.
Summary: Inflammatory activity appears to contribute to keratoconus development. Among 21 cytokines analyzed, 14 were found in higher concentrations in the tears of keratoconus patients compared to healthy individuals. IL-6 was notably elevated and correlated with disease severity. -
Keratoconus: an inflammatory disorder? – V Galvis, T Sherwin et al.
Summary: This review highlighted increased levels of interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-a), and matrix metalloproteinase-9 (MMP-9) in the tears of keratoconus patients, suggesting an inflammatory component to the disease. Eye rubbing, a known risk factor for keratoconus, was associated with elevated tear levels of MMP-13, IL-6, and TNF-a, indicating that mechanical trauma may contribute to the inflammatory response. -
Tear film inflammatory mediators in patients with keratoconus – Rana Sorkhabi, Amir Ghorbanihaghjo et al.
Summary: The study found that patients with keratoconus had significantly higher levels of Interleukin 6 (IL-6), Interleukin 1 beta (IL-13), and Interferon-gamma (IFN-y) in their tear film compared to normal controls. -
Cytokine Expression in Keratoconus and its Corneal Microenvironment: A Systematic Review – Robert Wisse, Jonas Kuiper, Renze Gan et al.
Summary: The review identified increased levels of pro-inflammatory cytokines, including interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-a), and matrix metalloproteinase-9 (MMP-9), in the tear film and corneal tissue of keratoconus patients. -
Serum inflammatory biomarkers are associated with increased choroidal thickness in keratoconus – João Pinheiro-Costa, Mário Lima Fontes et al.
Summary: The study suggests a relationship between increased choroidal thickness and inflammatory mechanisms in keratoconus patients. Elevated serum inflammatory indices — neutrophil/lymphocyte ratio (NLR), platelet/lymphocyte ratio (PLR), and systemic immune inflammation index (SII) — provide additional evidence of systemic inflammation's role in the development of keratoconus.
Copyright © 2025 | NETRA EYE INSTITUTE